Nasal or Face Mask? What’s Best for Neonatal Stabilisation?
- Published on:
Nasal or Face Mask? What’s Best for Neonatal Stabilisation?
- Published on:

On this page

The first moments after birth are critical for preterm infants, especially those born before 32 weeks’ gestation. Stabilising these fragile babies requires precise, gentle respiratory support. Traditionally, face masks have been the go-to interface for delivering positive pressure ventilation (PPV) and continuous positive airway pressure (CPAP) via a t-piece resuscitation circuit. However, nasal interfaces—such as prongs and masks—are increasingly being recognised for their potential benefits in reducing complications and improving outcomes during initial neonatal stabilisation.
Clinical Considerations
The European Consensus Guidelines on the Management of Respiratory Distress Syndrome (RDS) emphasise the importance of initiating non-invasive respiratory support from birth to reduce lung injury and bronchopulmonary dysplasia (BPD) [1]. While face masks are widely used, the guideline specifically highlights nasal interfaces as a potential alternative, due to evidence that suggests that face mask use may inadvertently trigger apnoea and bradycardia, particularly in spontaneously breathing infants [2].
Physiological Impact of Face Masks
The temporary apnoea and bradycardia seen, may be caused through triggering of the Trigeminocardiac reflex [2]. This is due to the placement of face masks over the mouth and nose which covers the area of the Trigeminal nerve. Stimulation of the Trigeminal nerve, through the need for caregivers to provide a seal and leak free interface between mask and baby, can provoke a Trigeminocardiac reflex, leading to sudden respiratory and hemodynamic changes such as breath-holding (apnoea), reduction of heart rate and changes in blood pressure [2].
In one study it was found that 29% of first-time face mask applications led to apnoea, compared to 8% during subsequent applications [3]. These results indicate the need for careful selection of interface type and gentle handling during neonatal stabilisation.
Using a Different Interface
A systematic review published in the ADC Fetal & Neonatal Edition compared nasal prongs/nasopharyngeal tubes with face masks during delivery room resuscitation. The findings showed no significant difference in mortality or major morbidities, but nasal interfaces were associated with lower rates of intubation and chest compressions, suggesting a gentler approach to stabilisation [4]. Couple this with the evidence that commonly available face masks are often too large for infants under 29 weeks’ gestation, potentially compromising seal and efficacy [5], while nasal prongs and nasal masks offer a more tailored fit, reducing the risk of air leaks and improving pressure delivery.
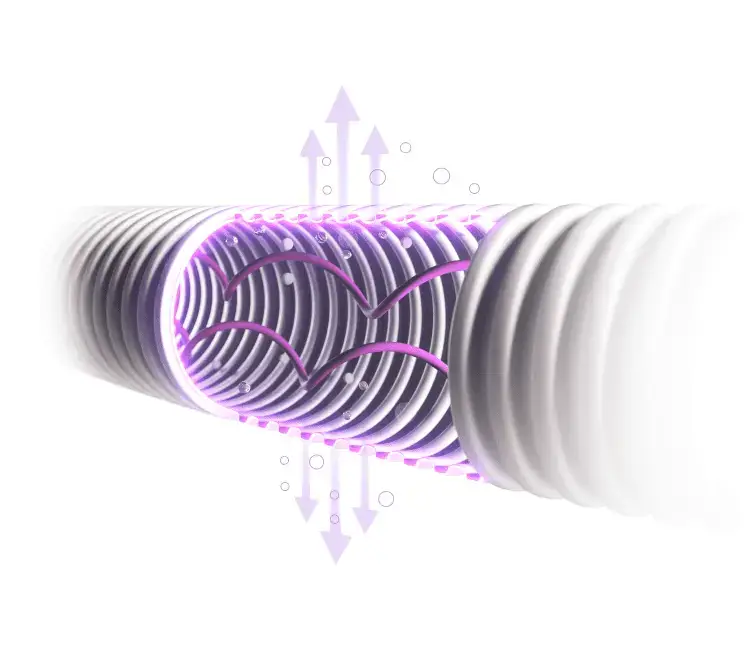
One such nasal interface product is the Inspire rPAP™ device. This two-piece device combines nasal prongs or face mask interfaces with fluidic flip nCPAP technology commonly seen in infant flow style nCPAP generators. The CORSAD randomised clinical trial demonstrated that using short binasal prongs with low work of breathing reduced delivery room intubation and mortality compared to standard face mask T-piece systems [6].

Inspire rPAP™

nCPAP generator
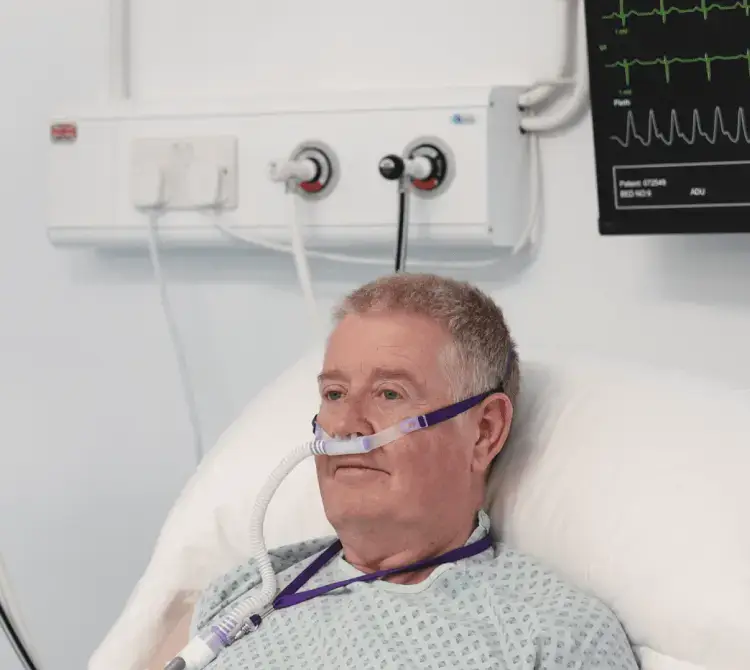
An alternative nasal interface stabilisation system is NeoFlow® Delivery Room CPAP (Eakin Respiratory). This product provides the ability to use common and standard delivery room equipment to apply known stabilisation principles via a nasal interface. The NeoFlow® Delivery Room CPAP product can seamlessly fit onto devices such as the Drager Resuscitaire, GE giraffe and Fisher and Paykel Neopuff so cost of capital equipment is removed. Available in 2.4m it has the additional benefit of easily facilitating respiratory support on the cord and enhanced delivery room cuddles.

NeoFlow® Delivery Room CPAP
Conclusion
While face masks remain a staple in neonatal resuscitation and stabilisation, emerging evidence supports the use of nasal interfaces—particularly prongs and nasal masks—for safer, more effective stabilisation of preterm infants. Innovations like NeoFlow® Delivery Room CPAP offer promising alternatives that align with modern guidelines and clinical needs.
As neonatal care continues to evolve, embracing interface technologies that reduce work of breathing, improve fit, and minimise physiological stress will be key to optimising outcomes for our smallest patients.

Emma Oduor
Neonatal Product Specialist
Specialising in Neonatal Products, I am passionate about helping healthcare providers and international partners gain an understanding of respiratory therapies for the tiniest of patients.
I believe in building strong and lasting partnerships with neonatal teams across the globe. I take great pride in helping them provide the best possible respiratory care for their patients and improving outcomes.

Emma Oduor
Neonatal Product Specialist
Specialising in Neonatal Products, I am passionate about helping healthcare providers and international partners gain an understanding of respiratory therapies for the tiniest of patients.
I believe in building strong and lasting partnerships with neonatal teams across the globe. I take great pride in helping them provide the best possible respiratory care for their patients and improving outcomes.